KNEE REPLACEMENT
Description
Knee replacement surgery (arthroplasty) is a routine operation that involves replacing a damaged, worn or diseased knee with an artificial joint.
Adults of any age can be considered for a knee replacement, although most are carried out on people between the ages of 60 and 80. More people are now receiving this operation at a younger age. A replacement knee usually lasts over 20 years, especially if the new knee is cared for properly and not put under too much strain.
Do I need a knee replacement?
In a healthy knee, the ends of your thigh and shin bones are covered with hard cartilage which allows the bones to move easily against each other. Arthritis damages the hard cartilage so that it becomes thin. In places the cartilage may wear away so that your bones rub against each other and become worn.
In a knee replacement operation, the worn ends of the bones and any remaining hard cartilage are removed and replaced with metal and plastic parts. The plastic acts like hard cartilage, helping your joint to move freely. The interlocking parts of the artificial joint allow your knee to bend while also making it more stable.
You won’t necessarily need a knee replacement if you have arthritis of the knee. But it may be worth considering if your knee is damaged by arthritis and the pain, disability or stiffness are having serious effects on your daily activities.
Even then, your healthcare team will always try other measures before suggesting a knee replacement, including drug treatments, physiotherapy and weight loss. If your symptoms are still manageable and your medication is effective then you may prefer to wait.
Your orthopaedic surgeon will be able to advise you on the surgical options and the potential pros and cons of having or delaying surgery, taking into account your age, health and level of activity.
Most people who have a knee replacement are over 60. The earlier you have a knee replacement, the greater the chances that you’ll eventually need further surgery. However, there’s evidence that the surgical outcome may be better if you don’t wait until your knee becomes very stiff or deformed.
Are there any reasons why I can’t have a knee replacement?
Unfortunately, some people may not be able to have a knee replacement even though their arthritis is very bad. This may be because:
• Your thigh muscles (quadriceps) are very weak and may not be able to support your new knee joint
• There are deep or long-lasting open sores (ulcers) in the skin below your knee, increasing your risk of infection.
What are the different types of knee replacement surgery?
There are several kinds of replacement knee joint as well as different surgical methods. Your doctor and orthopaedic surgeon should help you to choose the best option for you, taking into account the condition of your knee and your general health.
1. Total knee replacement
Most total knee replacement operations involve replacing the joint surfaces at the end of your thigh bone (femur) and at the top of your shin bone (tibia).
A total knee replacement may also involve replacing the under-surface of your kneecap (patella) with a smooth plastic dome. Some surgeons prefer to preserve the natural patella if possible, but sometimes the decision will need to be made during the operation.
If you’ve had a previous operation to remove the patella altogether (patellectomy), this won’t stop you having a knee replacement, but it may affect the type of replacement part (prosthesis) your surgeon uses.
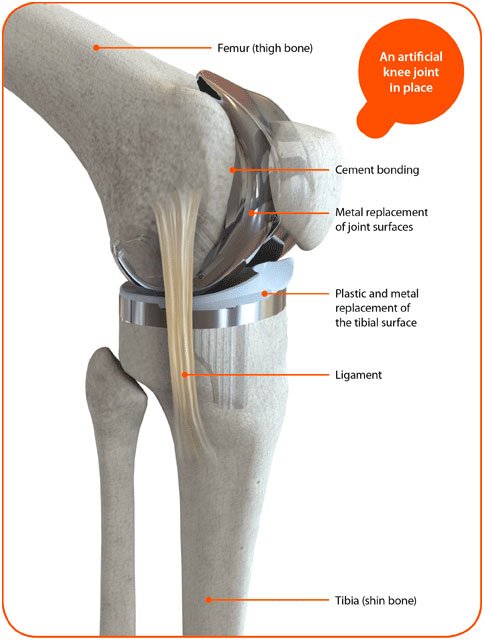
Total Knee Replacement
2. Unicompartmental (Partial) knee replacement
There are three compartments of the knee – the inner (medial), the outer (lateral) and the kneecap (patellofemoral). If arthritis affects only one side of your knee – usually the inner side – it may be possible to have a half-knee replacement (sometimes called unicompartmental or partial replacement). Because this involves less interference with the knee than a total knee replacement, it usually means a quicker recovery and better function.
Partial knee replacements can be carried out through a smaller cut (incision) than a total knee replacement, using techniques called reduced invasive or minimally invasive surgery. A smaller incision may further reduce the recovery time. Partial knee replacement isn’t suitable for everyone because you need to have strong, healthy ligaments within your knee. Sometimes this won’t be known until the time of surgery.
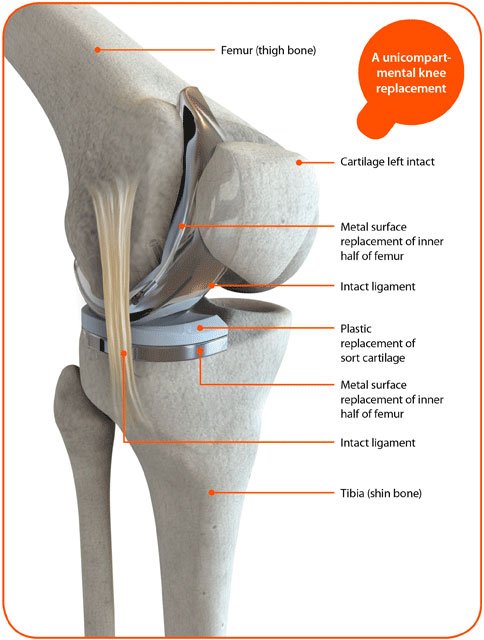
Unicompartmental Knee Replacement
3. Kneecap Replacement (Patellofemoral Arthroplasty)
It's possible to replace just the under-surface of the kneecap and its groove (the trochlea) if these are the only parts affected by arthritis. This is also called a patellofemoral replacement or patellofemoral joint arthroplasty.
The operation has a higher rate of failure than total knee replacement – which may be caused by the arthritis progressing to other parts of your knee. Some surgeons advise a total knee replacement as the results are more predictable. Others feel that it’s better to preserve the rest of the knee joint if it isn’t affected by arthritis.
The operation is only suitable for about 1 in 40 people with osteoarthritis. However, the outcome of kneecap replacement can be good if the arthritis doesn’t progress and it’s a less major operation offering speedier recovery times. More research is needed to understand which people are likely to do well with this operation.

Kneecap Replacement
4. Complex or Revision Knee Replacement
Some people may need a more complex type of knee replacement. The usual reasons for this are:
• major bone loss due to arthritis or fracture
• major deformity of the knee
• weakness of the main knee ligaments.
These knee replacements usually have a longer stem, which allows the component to be more securely fixed into the bone cavity. The components may also interlock in the centre of the knee to form a hinge to give greater stability. Extra pieces of metal and/or plastic may be used to make up for any removed or badly damaged bone. This type of operation may be needed if you’re having a second or third joint replacement in the same knee, and could be better from the start if you have very severe arthritis..

Complex Knee Replacement
What are the possible advantages of knee replacement surgery?
There are several possible advantages of knee replacement surgery. These include:
• freedom from pain
• improved mobility
• improved quality of life because everyday activities and exercise are easier.
Research has shown that four out of five people who've had knee replacement surgery are happy with their new knees. For those people who aren't happy, the main cause for dissatisfaction is continuing pain which may not be due to a problem with the operation. This is more of a risk if you have relatively minor joint damage (which may still cause severe symptoms) before surgery. If your joint damage isn't very severe it may be better to carry on with non-surgical treatments rather than risk a poor outcome from surgery.
What are the alternatives to knee replacement surgery?
Most doctors recommend non-surgical (conservative) treatments before considering a knee replacement. These include:
• diet - Losing weight will reduce the strain on your knee.
• exercise - Even though this may be difficult because of the pain, there's usually some form of non-impact exercise (for example swimming or cycling) that you can start gently and which will improve the strength and flexibility of your knee.
• drugs - Painkillers can reduce the pain in your joint, while non-steroidal anti-inflammatory drugs (NSAIDs) may help if your knee is swollen.
Pre & Post Pictures of Knee Replacement

Pre op Osteoarthritis knee grade 4

Post op Total knee Arthroplasty